What’s Holding Your Operating Room Back From Evaluating More Innovative Surgical Positioning Options?
Relying exclusively on contracts with Group Purchasing Organizations (GPOs) for patient positioning product selections may not yield the anticipated cost savings or performance benefits envisioned by the organization’s leadership and the C-Suite. Such strategies may also hinder the swift adoption of innovative solutions aimed at improving care and safety for both patients and caregivers. This is often due to the fact that these contracts tend to favor established vendors, thereby limiting the consideration of potentially superior alternatives. They also can fail to capture products and services that do not fit in commodity categories. Notably, the challenge intensifies when contracts for specific disciplines span from two to five years, further delaying the introduction of innovative products for surgical teams and patients.
It is crucial to understand that these organizations and their committees do not conduct clinical comparisons or verifications between products. They rely on relationships, administrative fees, and incentives to encourage customers to purchase contracted items. This pay-to-play system hinders the advancement of safety-focused innovations. While basic commodities like “Band-Aids and bedpans” may not evolve significantly over time and prioritize competitive pricing, many products directly influence the processes of clinical end users and the care they provide to their patients. These factors go beyond just cost. The concept of spreadsheet commoditization and a narrow focus on pricing fall short in the industry, particularly when clinicians are deprived of genuine comparative clinical value analyses. They are often conditioned to ask questions like: “are you on contract?” or “how much is it?”, instead of being provided with the necessary information for informed decision-making needed for choices that may not be available on contract. How can an organization who doesn’t provide hands on care, dictate product choices for clinicians? How are the least experienced people driving the decisions of those who are trained and educated to provide care? Why are GPO employees embedded in healthcare supply chains and on so called “Value Analysis Committees?”
Surgical positioning products should not be chosen based solely on price or brand recognition. Assuming they are all the same, including the processes needed for their use, can lead to poor ergonomic practices that hurt frontline caregivers. Before we came along, this industry thought it was perfectly acceptable to have surgical staff lift heavy patients with a lift sheet, to only then roll the patient back and forth to tuck the arms. A process that is practiced day in and day out in every operating room.
In fact, every major GPO and their so called “clinical” experts never even consider innovative improvements geared to provider safety, compliance with AORN standards, or even compliance with 10 state laws designed to protect the ergonomic safety of caregivers, in their product selections for contract. Their fees and share-backs were more important to them and their client’s C-suites than helping to evolve very well documented ergonomic impacts and injuries to their staff, something echoed in research articles all over the world. Happy to debate this statement in any public forum, anytime.
Sacrificing your personal safety, even that of your patient’s so others can benefit financially isn’t reducing the cost of care to society, no matter what GPOs say regarding their savings to the industry. One day soon, they will have to explain themselves in DC, and in courtrooms, as to how they conduct themselves with little oversight or accountability.
It is crucial to evaluate these products, or any product that impacts caregiver processes, through a comprehensive clinical value and utilization analysis to determine their true cost-effectiveness, performance, and ability to improve patient care and safety. While each contracted product may offer varying perceived values in terms of cost or performance, it is important to note that many were not primarily designed to enhance patient handling ergonomics in healthcare settings. Traditional systems require significant physical effort from clinical teams to reposition patients on surgical tables.
Drawing upon more than two decades of clinical anesthesia experience, our company has recognized a significant gap and felt compelled to innovate beyond the traditional methods of surgical positioning care. Throughout the United States, healthcare teams have encountered numerous challenges in patient handling and positioning, particularly with patient populations having high BMIs. Motivated by the need to address the observed inconsistencies and inadequacies in ergonomic processes, we embarked on developing the industry’s pioneering integrated patient handling and positioning platforms. These platforms are meticulously designed to enhance caregiver workflows and ensure ergonomic safety. Our unwavering commitment to this endeavor spans nearly a decade. Neglecting ergonomic safety, overlooking compliance with AORN safe patient handling standards, or disregarding state laws intended to safeguard the ergonomic well-being of surgical caregivers in favor of minimizing upfront costs or sticking to contracted products that do not tackle these crucial issues risks hindering progress in advancing patient care and safety.
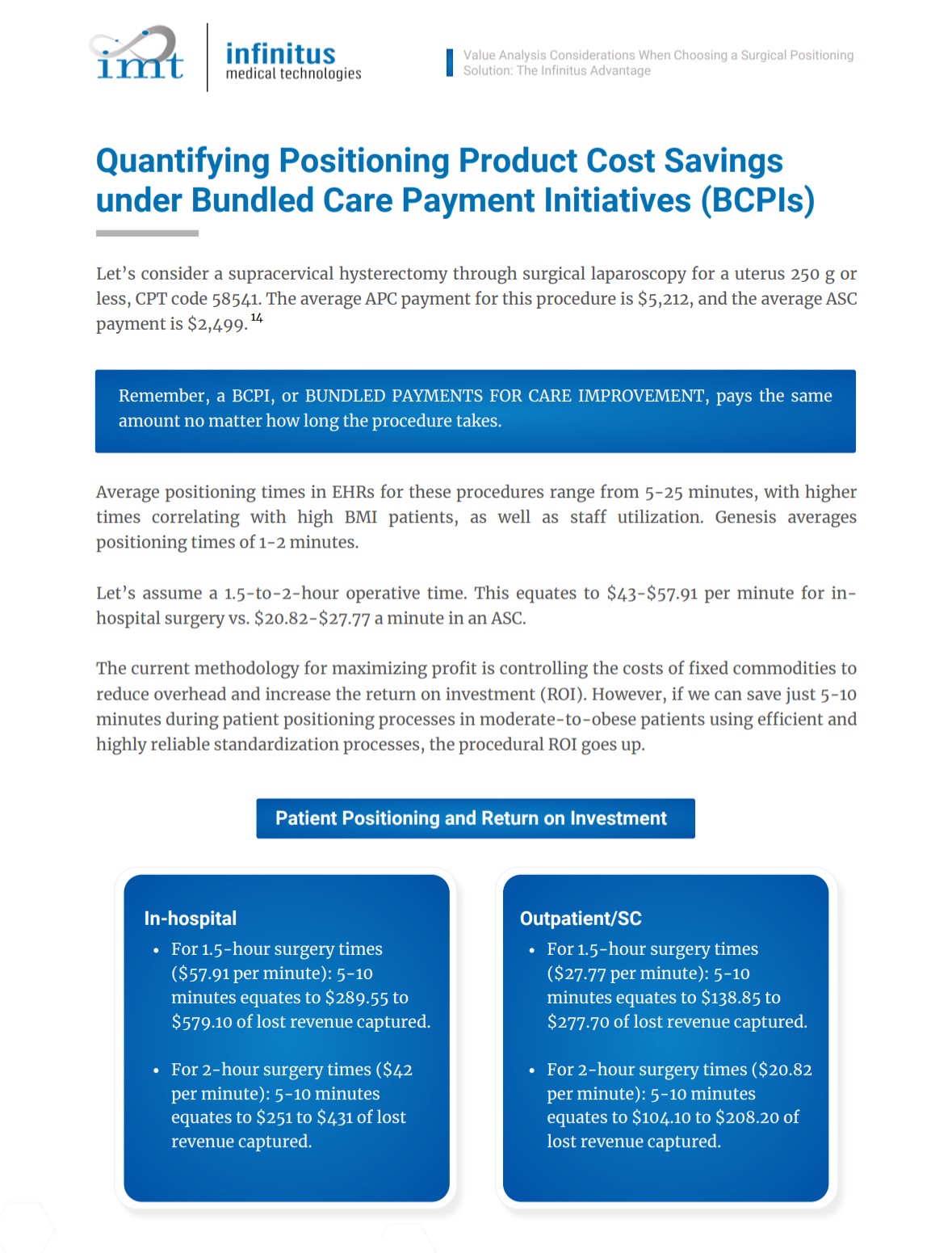
The responsibilities of caregivers and value analysis professionals extend beyond mere personal opinions and assumptions regarding product equality or performance. Their role is pivotal in ensuring that decision-making processes are guided by considerations that surpass simple contractual obligations and the idea of “cost”. It is essential for value analysis to look beyond price points and evaluate the broader implications of how products can influence performance, outcomes, and safety, even reimbursements under BPCIs. Neglecting to consider safer alternatives due to constraints imposed by supply chain limitations can impede advancements in healthcare for millions. Did you know it takes 10-15 years on average for innovations to reach the industry? These issues are the reason why.
Frontline caregivers possess a deep understanding of the challenges they face, challenges that may not be fully comprehended by group purchasing organizations (GPOs) or their compliant healthcare supply chain partners. GPOs frequently base their decisions on contractual agreements and quantitative analyses, without thoroughly considering the distinctive attributes of surgical positioning products. Furthermore, while GPOs might prioritize perceived costs and “kickback fees,†also known as “sharebacks,†they often overlook the clinical evaluation or comparison of the product options they mandate for healthcare providers. There is no clinical value analysis process comparing products on contract against each other. Happy to debate that anytime, anywhere, with anyone willing to challenge this statement in a live forum.
Neglecting critical value analysis and comparative processes, whether due to perceived cost implications or because the products are not under contract, represents a breach of the fiduciary duty of care that healthcare providers owe to their patients, as well as a risk to their own safety. It is crucial to equip caregivers with the knowledge required to make informed decisions that maintain the quality of care and safeguard the well-being of both patients and healthcare professionals.
While we acknowledge the rising costs of healthcare, it is important to understand that these costs are not inherently linked to the selection of superior or safer products from companies not on contract. Ironically, despite fixed healthcare cost markets overseas, there are far more superior product offerings and innovations created despite their reimbursement caps. Did you know that we are ranked 11th in healthcare innovation when compared to other nations?
Our healthcare costs are due to many factors, especially post Covid, but many of them stem from facilities overpaying for non-innovative commodities and taking “kickbacks†from companies under “Safe Harborsâ€, which are provided to both Group Purchasing Organizations (GPOs) and Pharmacy Benefit Managers (PBMs) by Congress, an exemption granted to only two types of entities in the entirety of the United States. In essence, your facilities may be receiving a “fee” directly from the company they are buying from under these contracts. This is not a reduction of price, which was the original intent of GPOs in pooling their resources for better scale and member pricing from selected vendors, it as evolved into companies outright paying for the opportunity to do business, while they keep competitive, even more innovative companies from coming into the market. Companies don’t just pay rebates without marking up the product. So ask yourself, who is actually getting the savings for your sacrifices?
We encourage providers to fight for choice and task your supply chains with allowing true clinical value analysis. Advocacy is the only way to evolve care and safety.