The Trendelenburg Chest Strap Myth: Are We Endangering Our Patients Due to Rigid Beliefs (DOGMA)?
In the surgical community, there’s a prevalent misconception that utilizing a chest strap to secure a patient in the Trendelenburg position negatively affects mechanical ventilation. This belief stems from the assumption that the strap binds the chest wall, thereby raising peak airway and inspiratory pressures during mechanical ventilation, which could elevate the risk of ventilator-induced lung injury (VILI). As a result, some medical facilities choose to forgo the use of these straps, which is at odds with the manufacturer’s guidelines for all foam-based Trendelenburg positioners available on the market. It’s important to note that while head and neck Trendelenburg systems may not necessitate the use of a strap, one is still required for lateral rotations of the surgical table.
While we advise against the use of tape or wide straps that may constrict large areas of the chest wall, a strap measuring 2-4 inches in width can be beneficial, especially when paired with a foam chest piece. This combination effectively mitigates direct pressure on the chest, lowering the risk of tissue injury while maintaining adequate ventilation. The foam chest piece promotes lateral expansion of the thoracic wall during mechanical ventilation by minimizing overall rigidity. Additionally, the strap is designed to wrap around the arms, facilitating lateral thoracic expansion as a result of mechanical ventilation.
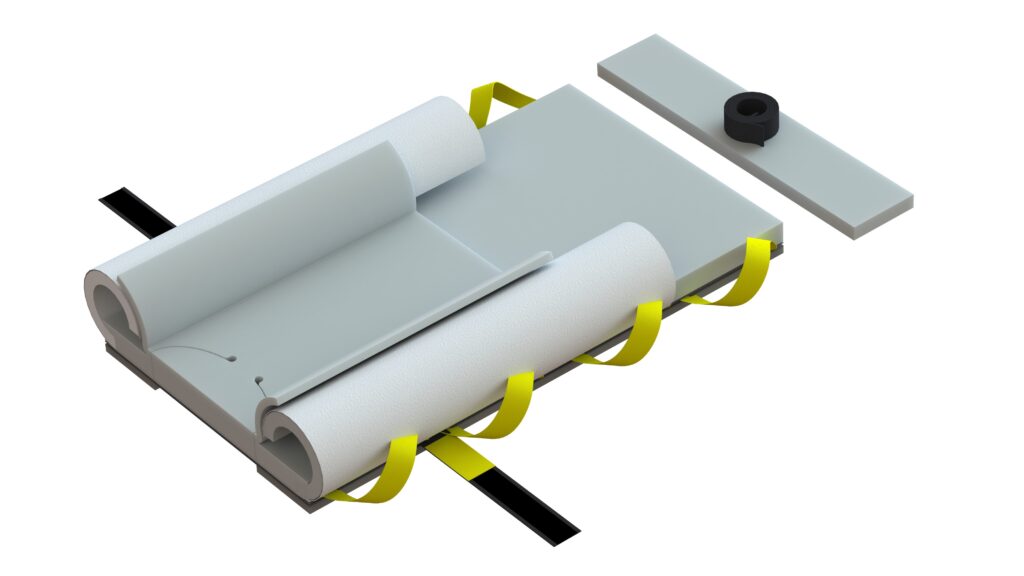
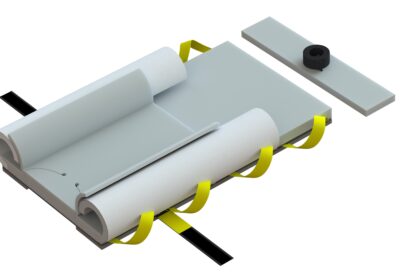
Genesis Bi-Wing AAP®
Three Straps vs Five:
Clinicians often ask why our Genesis Bi-Wing AAP® and Hadron FPLS® positioning systems do not include upper straps (featuring two distal straps and one chest strap for a total of three), especially when compared to our competitors’ standard four-strap, unreinforced foam systems, which still require an additional chest strap (totaling five straps).
Our design philosophy focuses on promoting highly reliable practices and compelled behaviors that enhance care standardization and patient safety. Human factors engineering is critical during research and development, as it emphasizes the processes involved and their impact on the overall desired outcome. When the goal is patient stability and safety, this focus makes it achievable. It’s actually easier to achieve. By standardizing the entire approach, we eliminate variations in patient handling and positioning processes, ensuring consistent outcomes each and every time. Successful patient positioning is the end result of a symphony of processes and caregiver roles. They must all be aligned to ensure patient and provider safety.
Unlike other unreinforced competitive foam-based Trendelenburg systems, our products are specifically designed with fabric-reinforced structural integrity, enabling them to lift and slide both the patient and pad together—supporting weights of several hundred pounds—even when used with mechanical lifts, without the risk of stretching or tearing.
Discover the three innovative ways we can safely move your patients without the need for draw or lift sheets!
Our two integrated distal straps are built into our patented FPLS® fabric foundation, ensuring that the patient and pad remain securely anchored to the surgical table during omnidirectional rotations. We intentionally exclude upper securing straps to encourage the use of the included chest pad and strap, which, along with the patient’s weight and the friction strips on the underside of the pad, effectively secures the upper portion of the pad to the table’s mattress and bed rail system. When utilized correctly, our systems achieve unsurpassed stability, with the straps and fused fabric reinforcing the foam’s foundation and integrity.
As the pioneers of reinforced foam pads and creators of the industry’s first combined patient handling and positioning platforms, our designs draw from over 20 years of experience in anesthesia and operating room environments. Our products have been on the market for nearly a decade and have been successfully used in tens of thousands of procedures, with no reported efficacy or safety issues. We specifically developed them to address over 20 years of entrenched dogmatic practices, process workarounds, and shortcuts that have historically compromised both staff and patient safety. Our innovative designs aim to restore balance and enhance safety in surgical environments. Most importantly, a chest strap is essential in securing the patient and the pad to the table. Ventilation issues arise not from routine strap use but from the degree and duration of the Trendelenburg angle required for the procedure. This is basic respiratory and pulmonary physiology, not a marketing claim.
Before we move on to the next section, please review this semi-brief video on gravity and physiology.
Having now established the vital role of the chest strap, let’s shift our focus to the physics of gravity-dependent positions and their relationship with mechanical ventilation. This is where we can dispel the misconception surrounding the use of a 2-4 inch chest strap and its effects on ventilation.
Back to Class: Respiratory Physiology
As surgical caregivers, we all possess a certain level of understanding of pulmonary physiology, but we often fail to fully appreciate its importance during the surgical positioning process. It’s crucial that we recognize and value these principles, as they play a significant role in ensuring optimal patient outcomes and safety.


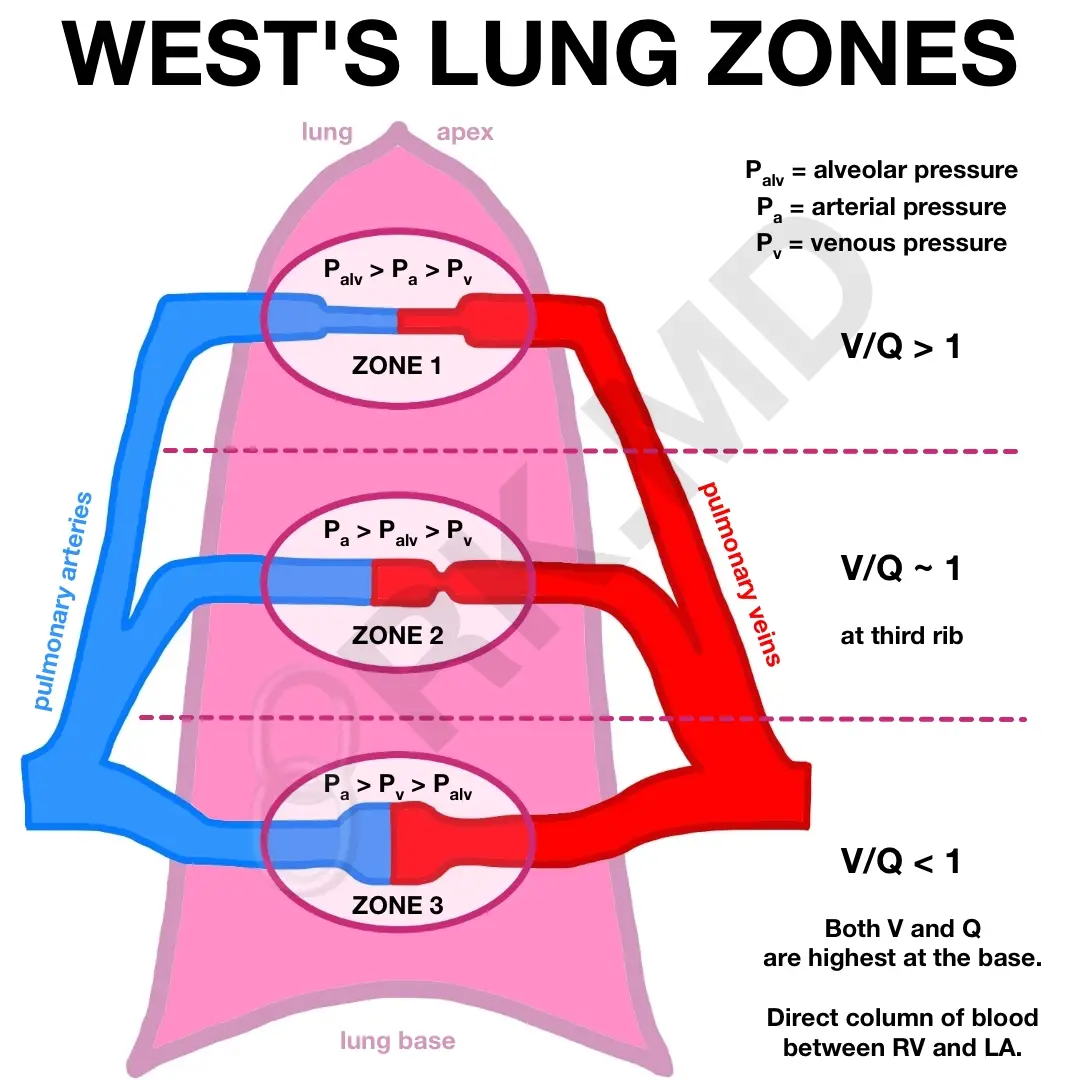
The above diagrams illustrate pulmonary physiology in a standing patient, with Zone 3 predominating in the supine position under normal conditions. This assumes intact autoregulation influenced by gravity and physiological responses. However, chronic lung conditions or obesity significantly alter these dynamics. For instance, morbidly obese patients exhibit higher closing volumes, chronic atelectasis, and reduced functional residual capacity, leading to faster desaturation during anesthesia induction.
In simple terms, pulmonary physiology involves the balance between circulation and air exchange. In general anesthesia, loss of autoregulation combined with gravity shifts causes ventilated air to follow the path of least resistance, often to areas with minimal circulation (dead zones), reducing effective oxygen uptake and carbon dioxide exchange. This is known as ventilation/perfusion (V/Q) mismatch. In a standing position, blood pools at the mid and base of the lungs, while the apex contains dead space with less air resistance due to reduced vascular space. Autoregulation plays a crucial role in maintaining the delicate balance of perfusion and gas exchange within the body when we are awake. When we are under general anesthesia, the following provides a clear path of understanding needed to keep our patients safe.
Pulmonary Physiology 101 (condensed):
Ventilation/perfusion (V/Q) mismatch refers to an imbalance between air reaching the alveoli (ventilation) and blood flow in the pulmonary capillaries (perfusion), impairing efficient gas exchange. In the Trendelenburg position—where the patient is tilted head-down, typically at 15-45 degrees—specific physiological changes exacerbate V/Q mismatch, particularly under general anesthesia.
Normal Pulmonary Physiology
- In a healthy, upright individual, gravity distributes blood flow preferentially to the lower (dependent) lung regions, while ventilation is more evenly distributed. This results in a V/Q ratio close to 1 in most lung zones, optimizing oxygen uptake and carbon dioxide removal.
- The lungs are divided into zones based on the relationship between alveolar pressure (PA), pulmonary artery pressure (Pa), and pulmonary venous pressure (Pv):
- Zone 1: PA > Pa > Pv (minimal perfusion, dead space, rare in healthy lungs).
- Zone 2: Pa > PA > Pv (intermittent perfusion).
- Zone 3: Pa > Pv > PA (best V/Q match, predominant in supine position).
- In the supine position, Zone 3 dominates, but gravity still influences regional blood flow and ventilation.
V/Q Mismatch in Trendelenburg
In the Trendelenburg position, the head-down tilt paired with losses in autoregulation alters the gravitational distribution of both ventilation and perfusion, leading to V/Q mismatch, especially under general anesthesia:
- Altered Ventilation:
- Gravity and Diaphragmatic Pressure: The head-down tilt causes abdominal contents to shift toward the diaphragm, increasing intra-abdominal pressure. This restricts diaphragmatic movement, reducing lung expansion, particularly in the dependent (lower, now cranial) lung regions.
- Reduced Functional Residual Capacity (FRC): The compression of the lungs decreases FRC, leading to atelectasis (alveolar collapse) in dependent regions. This reduces the volume of air available for gas exchange.
- Path of Least Resistance: Ventilated air preferentially flows to non-dependent (caudal, upper in Trendelenburg) lung regions where resistance is lower due to less compression. These areas may become over-ventilated relative to their perfusion, creating high V/Q ratios (akin to dead space).
- Altered Perfusion:
- Gravitational Blood Flow: In Trendelenburg, gravity directs blood flow toward the dependent (cranial) lung regions. These areas receive excessive perfusion, but due to atelectasis and reduced ventilation from diaphragmatic compression, gas exchange is impaired, creating low V/Q ratios (akin to shunt).
- Loss of Autoregulation: General anesthesia diminishes pulmonary vascular autoregulation (e.g., hypoxic pulmonary vasoconstriction), which normally redirects blood away from poorly ventilated areas. This exacerbates perfusion of poorly ventilated dependent regions.
- Resulting V/Q Mismatch:
- High V/Q Areas: Non-dependent (caudal) lung regions receive more ventilation but less blood flow, leading to wasted ventilation (dead space-like effect).
- Low V/Q Areas: Dependent (cranial) lung regions receive more blood flow but less ventilation due to atelectasis, leading to shunting where blood passes through the lungs without adequate oxygenation.
- This mismatch reduces overall gas exchange efficiency, causing hypoxemia (low blood oxygen) and hypercapnia (elevated carbon dioxide).
Aggravating Factors
- Obesity: Morbidly obese patients have higher intra-abdominal pressure and baseline atelectasis, further reducing FRC and worsening V/Q mismatch in Trendelenburg.
- Chronic Lung Disease: Conditions like COPD or pulmonary fibrosis disrupt normal V/Q relationships, amplifying mismatches.
- Anesthesia Effects: General anesthesia relaxes respiratory muscles and impairs autoregulatory mechanisms, increasing atelectasis and V/Q mismatch.
- Degree and Duration of Tilt: Steeper angles (e.g., >30 degrees) and prolonged time in Trendelenburg intensify diaphragmatic compression and atelectasis, worsening the mismatch.
Clinical Implications
- Hypoxemia: Reduced oxygenation due to shunting in dependent regions.
- Increased Airway Pressures: Mechanical ventilation may require higher pressures to overcome atelectasis, potentially elevating peak airway and inspiratory pressures.
- Ventilator-Induced Lung Injury (VILI): Excessive pressure or overdistension of non-dependent regions during mechanical ventilation can contribute to VILI, though this is more related to ventilator settings than the strap itself.
- Chest Strap Misconception: As noted in prior discussions, a properly designed 2-4 inch chest strap with foam does not significantly impair ventilation. V/Q mismatch in Trendelenburg is primarily driven by the angle and duration of tilt, not the strap, which is essential for patient security during table tilting.
Mitigation Strategies
- Optimize Ventilator Settings: Adjust I:E Ratios and various pressure setting modes as needed. Consider using positive end-expiratory pressure (PEEP) to prevent atelectasis and recruit collapsed alveoli in dependent regions.
- Minimize Tilt Angle and Duration: Limit the degree and time in Trendelenburg to reduce diaphragmatic compression.
- Positioning Aids: Use foam-based positioning systems (e.g., Genesis Bi-Wing AAP or Hadron FPLS) with chest straps and chest foam pieces to secure patients without significantly compromising chest expansion.
- Preoxygenation: Especially in obese patients, preoxygenation before induction can delay desaturation. Always place the patient close to anesthesia during airway management and intubation. This is exactly why our Genesis and Hadron systems were designed almost a decade ago!
- Monitoring: Continuous pulse oximetry and capnography to detect and manage hypoxemia or hypercapnia early.
Summary
In Trendelenburg, V/Q mismatch arises from gravity-driven shifts in ventilation and perfusion, compounded by diaphragmatic compression, atelectasis, and anesthesia-related loss of autoregulation. Dependent lung regions become under-ventilated but over-perfused (low V/Q, shunt-like), while non-dependent regions are over-ventilated but under-perfused (high V/Q, dead space-like). This leads to impaired gas exchange, particularly in obese patients or those with lung disease. The degree and duration of the tilt, not the use of a properly designed chest strap, are the primary drivers of these effects. Proper positioning, ventilator management, and minimizing tilt can mitigate V/Q mismatch. All of these physiological issues impact ventilation more than a chest strap.
For Anesthesia:
Here are some general ventilation strategies for patients undergoing Trendelenburg required procedures. Please research your own policies and literature surrounding research in this area. The following general guidelines incorporate the research and strategies suggested in the ARDSnet protocol (NIH NHLBI ARDS Clinical Network). They are only suggested guidelines and not a protocol from infinitus Medical Technologies.
Mechanical ventilation in the Trendelenburg position—where the patient is tilted head-down—poses unique challenges due to increased intra-abdominal pressure, reduced functional residual capacity (FRC), atelectasis, and ventilation/perfusion (V/Q) mismatch. These factors can elevate the risk of ventilator-induced lung injury (VILI), characterized by barotrauma (high pressure), volutrauma (overdistension), atelectrauma (repetitive alveolar collapse), and biotrauma (inflammation). Below are evidence-based mechanical ventilation techniques to minimize lung injury in patients positioned in Trendelenburg, particularly during surgical procedures under general anesthesia.
Key Techniques to Reduce Lung Injury
- Low Tidal Volume Ventilation (Protective Lung Strategy)
- Rationale: High tidal volumes can overdistend alveoli, causing volutrauma, especially in non-dependent lung regions in Trendelenburg where ventilation is preferentially directed.
- Implementation:
- Use tidal volumes of 6-8 mL/kg of predicted body weight (PBW) to avoid excessive stretch.
- Monitor plateau pressures (Pplat) and keep them below 30 cmH₂O to minimize barotrauma.
- Trendelenburg Consideration: The head-down position reduces FRC, increasing the risk of atelectasis in dependent regions. Low tidal volumes prevent overdistension of non-dependent areas while used in conjunction with other strategies to address atelectasis.
- Evidence: The ARDSNet protocol demonstrated reduced mortality with low tidal volume ventilation in acute respiratory distress syndrome (ARDS), and these principles are applied to non-ARDS patients to prevent VILI.
- Positive End-Expiratory Pressure (PEEP)
- Rationale: PEEP prevents alveolar collapse (atelectrauma) in dependent lung regions, which are prone to atelectasis in Trendelenburg due to diaphragmatic compression from abdominal contents.
- Implementation:
- Apply moderate PEEP (5-10 cmH₂O, adjusted based on patient characteristics like obesity or lung compliance).
- Titrate PEEP to maintain adequate oxygenation (SpO₂ ≥ 88-92%) without compromising hemodynamics, as excessive PEEP can reduce venous return in Trendelenburg.
- Use recruitment maneuvers cautiously (e.g., brief periods of high PEEP or sustained inflation) to open collapsed alveoli, followed by optimal PEEP to keep them open.
- Trendelenburg Consideration: Higher PEEP may be needed in obese patients or those with prolonged Trendelenburg positioning to counteract atelectasis, but careful monitoring is required to avoid barotrauma or cardiovascular compromise.
- Evidence: Studies show PEEP reduces atelectasis and improves oxygenation in surgical patients, particularly in steep Trendelenburg (e.g., robotic surgeries).
- Recruitment Maneuvers
- Rationale: Recruitment maneuvers temporarily increase airway pressure to open collapsed alveoli, improving ventilation distribution and reducing V/Q mismatch.
- Implementation:
- Perform maneuvers sparingly (e.g., 30-40 cmH₂O for 20-30 seconds or stepwise increases in PEEP) to avoid hemodynamic instability or barotrauma.
- Follow with adequate PEEP to maintain alveolar patency.
- Avoid in patients with contraindications (e.g., high intracranial pressure, hemodynamic instability).
- Trendelenburg Consideration: Dependent lung regions are prone to collapse in Trendelenburg, making recruitment maneuvers useful, but the head-down position increases intracranial and intraocular pressure, necessitating caution.
- Evidence: Recruitment maneuvers improve intraoperative oxygenation in Trendelenburg, particularly in obese patients, but benefits must be weighed against risks.
- Pressure-Controlled Ventilation (PCV) or Volume-Controlled Ventilation (VCV) with Pressure Limits
- Rationale: PCV limits peak airway pressures, reducing barotrauma risk, while VCV with pressure caps ensures consistent tidal volumes without excessive pressure.
- Implementation:
- In PCV, set inspiratory pressure to achieve tidal volumes of 6-8 mL/kg PBW while keeping Pplat < 30 cmH₂O.
- In VCV, use a decelerating flow pattern and set pressure alarms to avoid high peak pressures.
- Monitor for auto-PEEP (incomplete exhalation), which can occur in Trendelenburg due to reduced lung compliance.
- Trendelenburg Consideration: The increased intra-abdominal pressure in Trendelenburg reduces lung compliance, making PCV advantageous for maintaining stable pressures, though VCV is also effective with proper settings.
- Evidence: Both modes are effective in surgical settings, with PCV often preferred in low-compliance states like Trendelenburg.
- Optimize Respiratory Rate and Inspiratory:Expiratory (I:E) Ratio
- Rationale: Proper respiratory rate and I:E ratio maintain adequate minute ventilation and prevent hypercapnia while avoiding air trapping or overdistension.
- Implementation:
- Set respiratory rate (12-20 breaths/min) to achieve normocapnia (PaCO₂ 35-45 mmHg).
- Use an I:E ratio of 1:2 or 1:3 to allow sufficient expiratory time, reducing the risk of auto-PEEP.
- Adjust based on capnography and arterial blood gas results.
- Trendelenburg Consideration: Reduced lung compliance and atelectasis may require higher respiratory rates to maintain ventilation, but excessive rates can cause air trapping, particularly in obese patients.
- Evidence: Balanced ventilation settings reduce VILI risk in intraoperative settings.
- Minimize Oxygen Toxicity
- Rationale: Prolonged exposure to high fractional inspired oxygen (FiO₂) can cause oxidative stress and lung injury.
- Implementation:
- Use the lowest FiO₂ to maintain SpO₂ ≥ 88-92% (typically 0.4-0.6 in healthy lungs).
- Combine with PEEP and recruitment maneuvers to improve oxygenation without relying on high FiO₂.
- Trendelenburg Consideration: V/Q mismatch in Trendelenburg may tempt clinicians to increase FiO₂, but this should be avoided in favor of optimizing ventilation strategies.
- Evidence: Lower FiO₂ with protective ventilation reduces oxidative lung damage.
- Individualized Ventilation for High-Risk Patients
- Obese Patients:
- Use higher PEEP (10-15 cmH₂O) to counteract reduced FRC and atelectasis.
- Adjust tidal volumes based on PBW, not actual body weight, to avoid overdistension.
- Consider slight reverse Trendelenburg (if surgically feasible) to reduce diaphragmatic compression.
- Patients with Lung Disease:
- Tailor PEEP and tidal volumes to lung compliance (e.g., lower tidal volumes in restrictive diseases like pulmonary fibrosis).
- Avoid high pressures in obstructive diseases (e.g., COPD) to prevent air trapping.
- Trendelenburg Consideration: Obese patients and those with lung disease are particularly vulnerable to V/Q mismatch and atelectasis in Trendelenburg, requiring careful titration.
- Evidence: Individualized strategies improve outcomes in high-risk surgical patients.
- Obese Patients:
Additional Considerations in Trendelenburg
- Chest Strap Use: As discussed previously, a 2-4 inch chest strap with foam does not significantly impair ventilation. Misconceptions about straps causing VILI are unfounded; the degree and duration of Trendelenburg tilt are the primary drivers of lung injury risk.
- Minimize Tilt Angle and Duration: Limit the angle (e.g., <30 degrees) and duration of Trendelenburg to reduce diaphragmatic compression and atelectasis, which exacerbate V/Q mismatch and VILI risk.
- Monitoring:
- Use continuous pulse oximetry, capnography, and intermittent arterial blood gases to monitor oxygenation and ventilation.
- Track plateau pressures, driving pressures (Pplat – PEEP, ideally <15 cmH₂O), and tidal volume compliance to detect early signs of lung stress.
- Preoperative Optimization: Preoxygenation with 100% FiO₂ for 3-5 minutes before induction, especially in obese patients, delays desaturation and supports initial ventilation.
Summary
To reduce lung injury in Trendelenburg, employ low tidal volume ventilation (6-8 mL/kg PBW), moderate PEEP (5-10 cmH₂O), and selective recruitment maneuvers to prevent atelectasis and overdistension. Use pressure-controlled or volume-controlled ventilation with pressure limits, optimize respiratory rate and I:E ratio, and minimize FiO₂ to avoid oxygen toxicity. Tailor strategies for high-risk patients (e.g., obese or those with lung disease) and minimize Trendelenburg angle and duration. Proper positioning with chest straps and foam supports safe ventilation without contributing to VILI. Continuous monitoring ensures early detection of complications, aligning ventilation with the patient’s physiological needs. Always review all current literature and research on ventilation strategies and management, as these can change over time.
Allow us to demonstrate why we are the leading surgical positioning company in the industry. Our focus is on education and process optimization, achieved through innovative design and extensive clinical experience. This commitment is what enables us to consistently outpace and outperform our competitors.
We have always dedicated our efforts to balancing patient and surgical caregiver safety: infinitusmedical.com.