Evolving Surgical Positioning and Pressure Management: Arm Adduction, Part 2

Processes should always serve as the foundation for patient positioning research and development, ensuring that providers are not compelled to adapt inadequate procedures to make their products work. While many claim to enhance surgical or patient care safety, it is essential to acknowledge that staff safety is the cornerstone for improving overall processes necessary to achieve this goal.
Group Think and Belief in Inherent Morality of the Group: “I had the distinct feeling that we were in the position of having to prove that it was unsafe instead of the other way around.â€
When we combine these advancing surgical platforms with highly diverse “one size fits all” infrastructure or comorbidities such as adult obesity, an emerging risk to everyone in the operating room becomes apparent. Mitigating these risks necessitates improving our processes and clinical understanding of the controllable factors, and then seeking solutions that reinforce these principles.
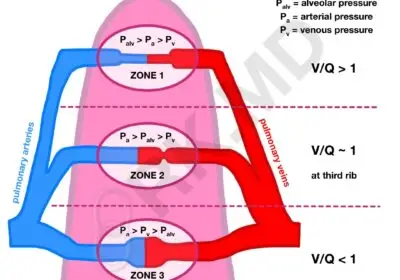
Pressure injury risks and realities are intricate and multifaceted. While we can certainly delve into the physiological and co-existing morbidities that contribute to higher patient risks for pressure injuries in the operating room, as well as strategies to optimize screening and anesthesia management for their reduction, such discussions warrant a separate article. For now, let’s keep it concise. However, before we conclude this topic, a word of caution: exercise caution when interpreting pressure mapping data presented in marketing materials. It can be misleading. Was it measured against a hard surface or a soft surface? Considering the fact that we place various items with different firmness scales under the patient, it is certain that transmural pressures are not consistent and should always be taken into account.Â
This is precisely why we directly measure our technologies on hard surfaces. Additionally, temperature to pressure gradients exist when using memory-type foams, as they undergo the glass transition phase. Their chemical composition exhibits reduced viscosity in colder environments like the operating room, where they rely on direct warmth from the patient to function as intended.
The objective is to briefly highlight areas in which we can evolve through a multipart series focused on specific topics. In each article, we will elucidate historical methods and then contrast them with process-oriented solutions to facilitate progress. This particular article will address the evolving arm adduction processes necessary to impact the care and safety of patients and surgical caregivers alike.
Evolving Positioning Standards: Arm Adduction
Most laparoscopic procedures performed today require some form of arm adduction. Over the past 18 years of practicing anesthesia, we have observed a shift in most cases, necessitating either unilateral or bilateral arm adduction. This shift can largely be attributed to the limited <90 degree space between an abducted arm position and the surgical table. This relatively confined area restricts proximal access to the surgical field for the surgical teams, especially when combined with the placement of commonly used instruments and infrastructure. Robots often come to mind in this context.
If we examine the historical diagrams (such as the one below) that illustrate traditional weight-based circumferential wrapping of the arms with a sheet, we may notice one significant aspect: these methods always assume that the patient fits on that 20-21 inch wide surgical table. Considering that almost 40% of the adult population in the United States has a BMI exceeding 30, it becomes apparent how this outdated standard can quickly devolve into a highly variable process.
Traditional patient weight based circumferential arm adduction requires a great deal of ergonomic effort from the staff. If they also have to move the patient into a position like lithotomy, you begin to see that the reliance on a lift sheet has severe limitations.
If you are placing your patients in Trendelenburg for example, the sheet actually impedes optimized pad to skin contact needed for stability, after all it’s the combined skin to surface contact that creates the friction coefficient needed for optimized traction and stability. Do teams want 20-40% of effective pad to skin contact or do they want 100%? It’s not a marketing ploy, it physics!
Certain facilities may attempt to bypass the process by placing a sheet under a foam or gel top to optimize pad-to-skin contact. However, regrettably, this approach proves counterproductive and undermines the intended outcome. Ultimately, the sheet still ends up back under the patient, negating the desired skin contact surface preservation.
This can be regarded as a failure in the adaptive process, as it introduces instability at two levels: between the patient and the pad or gel surface, and the friction surface between the gel or foam pad and the mattress top, which is crucial for maintaining the pad’s structure and integrity. If a foam-based Trendelenburg system is used, nothing should ever be inserted between the mattress and foam surface, as this violates the manufacturer’s instructions for use (IFU) and places liability at the user’s risk. It exemplifies a workaround process.
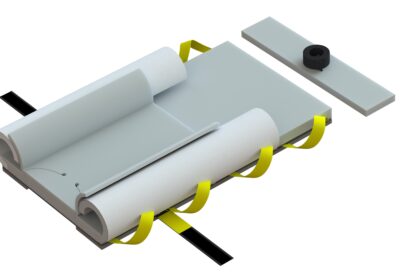
Most foam pads incorporate sewn-in straps with limited structural integrity to reinforce them. If these straps move due to reduced surface contact with the mattress or during patient/pad movements (e.g., in steep Trendelenburg), they may elongate and tear. This is a consequence of the material characteristics. When transferring patients to lithotomy, for instance, healthcare staff must physically lift the entire patient from a high friction coefficient surface. Anything less than this can pose difficulties, such as pad bunching or tearing, as demonstrated in the accompanying video.
Certain institutions attempt to optimize the contact surface between padding and skin by reducing the size of the lift sheet. Can you imagine the challenge of lifting a patient into lithotomy position with a six-inch draw sheet? Would such a small draw sheet adequately support the entire arm in case of arm adduction? Absolutely not. This serves to illustrate the alternative methods employed by surgical staff due to the limitations of a one-size-fits-all approach that fails to consider the unique patient handling and positioning processes of each staff member.
It is crucial for patient positioning companies to comprehend the workflow processes of surgical teams and develop solutions that optimize them.
Before we move on, I must caution against the inappropriate use of “hover-style” patient transfer products placed between foam Trendelenburg positioning systems and the mattress. This should never occur. While these products are exceptional for lateral transfers, when placed beneath a foam pad specifically designed for direct contact with the mattress, the consequences can be disastrous. They possess a low friction coefficient meant to facilitate easy sliding. Consequently, placing a low-friction device under a surface that requires a high friction coefficient may result in sliding, foam tears, and falls from the table. If anyone doubts this, I would be delighted to connect them with reliable sources that have documented such incidents. This represents one of the most concerning examples of workarounds compromising patient safety. Near falls and patient falls from the surgical table occur far more frequently than people are willing to acknowledge.
Wrapping the arms is not as simple as using a mere sheet; some form of padding is necessary to alleviate pressure. Additionally, comprehensive arm support off the sides of the table is required. Personally, we advocate for foam and here’s why: gel does not expand to accommodate natural third-spacing or gravity-dependent edema formation. Instead, it exerts pressure back into the tissue rather than outward. While gel proves beneficial for pressure management, its material characteristics entail risks when circumferentially wrapping the arms. A prominent US institution even employed a pressure sensor to monitor pressure increases when using gel wraps during arm adducted cardiac procedures, following a series of questionable injuries. We eagerly await the publication of their findings.
Conversely, wrapping the arms in foam allows for the necessary expansive properties to compensate for spatial changes during tissue expansion, while providing the appropriate rebound and support for pressure management.
However, it is important to bear in mind that all the sheets, foam, gel, tape, sleds, and other methods employed to secure the arms also impede anesthesia access. Collectively, they heighten the risk of compartment syndrome. Fortunately, our products and methodologies obviate the need for these processes or workarounds.
One additional note to consider when using weight based circumferential arm adduction: Lateral rotation of the table creates a tourniquet effect on the down arm, as the patient slides and tightens the sheet placed under them and around the arm during the gravity shift of weight. This increases the risk for compartment syndromes.
If you or your surgical teams would like any additional information on how we can drive high reliability in your surgical practice, please contact us today. We know this space as a clinically founded and run company. We understand your challenges!