Evolving Surgical Positioning and Pressure Management: Arm Adduction, Part 1

Surgical patient positioning is a meticulous daily practice observed in operating rooms worldwide. However, as modern surgical platforms continue to advance, it is worth considering whether the surgical industry has kept pace in evolving surgical positioning techniques and standards.
Patient handling and positioning procedures, akin to surgical care, necessitate ongoing progress and refinement. Just like our patients, these processes are nuanced and exhibit individuality to some degree. It is imperative for caregivers to constantly evolve and explore novel approaches to ensure the safety of both patients and colleagues during these tasks. This should never be a standardized process solely focused on cost considerations within the supply chain.
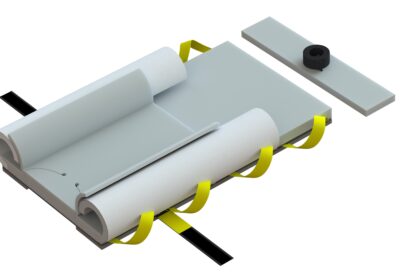
This series presents several noteworthy aspects to contemplate when selecting appropriate solutions for surgical teams, with a primary emphasis on patient well-being. These issues are mutually dependent and yet exclusive to all individuals in the operating room. Striking a balance between safety and patient handling is always crucial.
Historical Processes and Methodologies
As an industry, it is essential to acknowledge that many of our surgical positioning processes and guidelines are outdated. They have failed to keep up with the advancements in surgical platforms such as minimally invasive laparoscopic platforms, robotic technologies, and the rapid changes in patient co-morbidities. Additionally, newer orthopedic platforms designed for anterior hip procedures should equally be considered, although those topics will be addressed in a subsequent article.
While these examples demonstrate the progress in procedural surgical care, they all share a common characteristic: each platform requires specialized patient handling and positioning requirements.
All of them subject our patients to higher degrees of sheer force, inertial movements into fixed structures, and a wide range of gravity-dependent surgical table positioning demands, each with some physiological impact or risk of injury.
The current patient handling and positioning processes in this industry exhibit high variability from one institution to another and from one surgeon to another. These processes are labor-intensive and often involve poor ergonomic patient handling practices, increasing musculoskeletal disorder (MSD) risks for surgical staff. To prioritize the safety of surgical staff, many teams are compelled to develop workarounds that sometimes compromise the safety of patients, particularly when caring for high BMI patients. Some of these cultural practices result from the acceptance of “Normalization of Deviance” and “Group Think.” While these acceptances have impacted the safety of global aviation and space programs, particularly in the United States, they have also found their way into the healthcare lexicon.
As a company owned by Veterans and with experience in naval aviation and flight deck operations, as well as nearly two decades in the operating room, we have consistently prioritized product design that minimizes variance through high reliability. Variance undermines accountability and compromises the mission’s success.
Normalization of Deviance And the Dangers of Groupthink
There’s a natural human tendency to rationalize shortcuts under pressure, especially when nothing bad happens. The lack of bad outcomes can reinforce the “rightness†of trusting past success instead of objectively assessing risk.Â
For instance, when lithotomy is necessary for surgical care, most teams commonly aim to minimize the lifting and movement of anesthetized patients by positioning them in a lithotomy-ready stance. However, this approach compromises the anesthesiologist’s access to the airway and subsequent management required for general anesthesia. As a result, anesthesia providers are compelled to reach an average distance of 7-14 inches to effectively manage the airway and perform intubation. Particularly during the Covid-19 pandemic, this poses a significant risk, as limited access to ensuring a proper mask seal or delays in expediting a prompt laryngoscopy can increase the potential for aerosolized droplet spread to all individuals in the room. The same applies to extubation.
This practice, known as the “normalization of deviance,” is unfortunately prevalent in daily operations. “It’s just the way we have always done it!”
It is crucial for surgical teams to recognize that all of our positioning procedures have an impact on other caregivers in the operating room. Therefore, the development of highly reliable processes is imperative as they enhance the safety, efficacy, performance, and accountability of the entire team.
If you or your surgical teams would like any additional information on how we can drive high reliability in your surgical practice, please contact us today. We know this space as a clinically founded and run company. We understand your challenges!